PrEP: Preventative HIV drug highly effective, study says

A drug which stops HIV infecting the body has proved to be a highly effective “real-world” preventative treatment, a study has confirmed.
The results of the research on 24,000 people taking it across England, have been described as “reassuring”.
Thousands of people are already taking PrEP through sexual health clinics.
HIV charity the Terrence Higgins Trust wants easier access to the drug, since many people, including women, do not know it exists.
The UK Health Security Agency (UKHSA), which led the PrEP Impact Trial with the Chelsea and Westminster Hospital NHS Foundation Trust, said it was the largest ever real-world study of its kind.
It was carried out at 157 sexual health clinics across England between October 2017 and July 2020.
The study found use of PrEP, also known as pre-exposure prophylaxis. reduced the chances of getting HIV by 86%. Clinical trials suggested it was 99% effective.
Dr John Saunders, a consultant in sexual health and HIV who worked on the study, said: “This trial has further demonstrated the effectiveness of PrEP in preventing HIV transmission and has, for the first time, shown the protective effect reported by earlier trials, but at scale, and delivered through routine sexual health services in England.”
The Terrence Higgins Trust HIV charity welcomed the study’s publication, but said there was “more to be done” to increase access to, and awareness of, the drug, particularly among some minority groups.
Debbie Laycock, head of policy, said: “We think that there are certain communities and individuals at the moment who could benefit from PrEP but aren’t accessing it.”
“Many women just don’t know PrEP exists,” she added.
She said the charity was calling for PrEP to be made available in pharmacies and online to widen access to it.
Dr Saunders said that although the clinical success of the drug had been proven, this study revealed other important information about how it is used.
“Before, we didn’t know how many people would want it, take it, or how long they would stay on it for,” he said.
“Now we know who is being prescribed it and we can work with clinics to try and get more people to take it.”
He said that “real-world effectiveness” was dependent on many factors, particularly whether the drug is taken correctly.
‘Liberating’
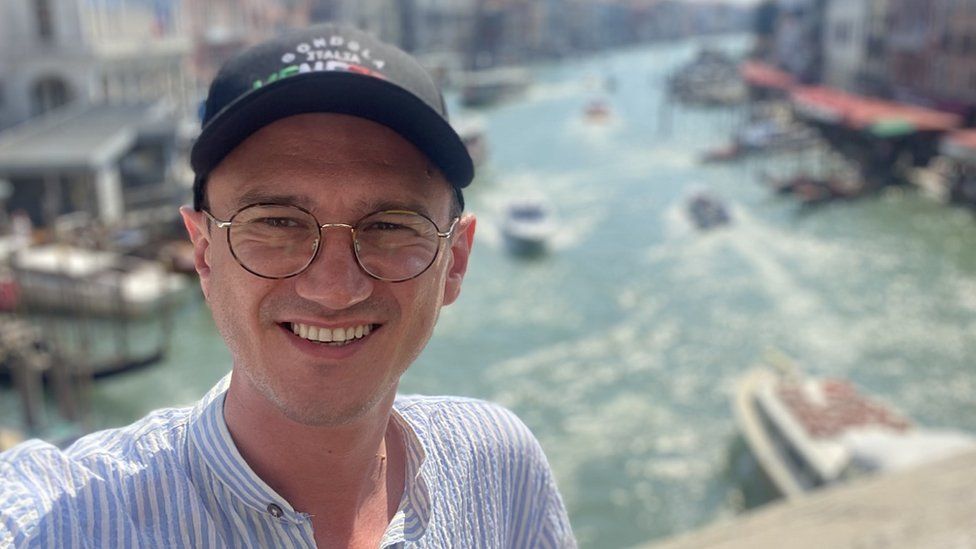
Harry Dodd, who has taken part in several PrEP trials, said taking the drug has been “empowering” for him as he no longer fears catching HIV.
“I haven’t thought about that for the best part of a decade and that’s liberating. I have had long-term partners who have HIV since [taking the drug] and that would not have been on my radar before. I now have the confidence to love freely.”
However, Mr Dodd, 33, from north London, said he believed there was a “stigma” attached to the drug as it was “sexually related and historically connected to gay communities”.
The UKSHA said the effectiveness of the drug would help achieve the government’s aim of zero HIV transmissions by 2030, but that more people needed to take it.
Dr Saunders said that while gay and bisexual men were most likely to use the drug, many people from other groups, such as straight women, would benefit from taking it.
PrEP, which contains existing HIV treatment drugs tenofovir disoproxil and emtricitabine, works by stopping HIV from entering the body and making copies of itself.
It can either be taken as a daily pill or an “event” basis before sexual intercourse.
The decision to make the treatment widely available on the NHS in England in 2020 was partly based on earlier findings from this research, as well as results of earlier clinical trials.
The results of this study, published in the Lancet HIV, have only just been released because of the large sample size and the time taken to peer review it.